This blog includes highlights and key points from the article Service re-design in healthcare: the impact of innovative methods to compare costs and benefits (Anderson et.al, 2019).
The article was written by Robyn Millar, Gillian H. Anderson (corresponding author) Robert Van Der Meer and Alec Morton – all at the Department of Management Science, University of Strathclyde Business School
In the face of growing cost pressures, policy makers are looking for cost effective ways to meet the increasing healthcare needs of the population and improve the service to patients[1].
The collaborative study between the University of Strathclyde, The Scottish Government and NHS Scotland seeks to demonstrate the cost effectiveness of an innovative ‘virtual’ patient pathway – and, more generally, supported capacity building in service redesign and improvement across the Scottish health service.
To the authors knowledge, this is the first time that discrete event simulation has been used in an action research approach to develop bottom-up micro costing models to evaluate the kind of virtual clinic approach that is rapidly gaining acceptance in NHS Scotland and beyond[2].
Policy context
In 2018, the auditor general for Scotland claimed that the NHS was not financially stable in its current form, with pressure building in several keys areas such as rising drug costs and a significant maintenance backlog.
The authors suggested that to effectively cope with the problem of improving Scottish healthcare in a sustainable manner, new service models must be designed and tested that are clinically effective and cost effective and also patient friendly.
One of the key challenges faced by NHS Scotland over the past decade is a substantial increase in the volume of outpatient appointments.
According to a 2017 report from the Scottish Government, NHS Scotland delivers around 4.5 million outpatient appointments on an annual basis, which represents a total increase of over 140,000 patients when compared to 2009[3].
But, not all of these outpatient appointments may be necessary. In the annual report for 2017-18, the Chief Medical Officer for Scotland recommended that outpatients should be seen face-to-face only if it is in their best interest or if they prefer it, highlighting the introduction of ‘opt-in’ clinical helplines and ‘virtual clinics’ as a practical approach to reduce unnecessary outpatient attendances.
The authors also recommend that virtual clinics should be designed to conform to the core principles of the Scottish Access Collaborative Programme[4], created by the Scottish Government to sustainably improve patient waiting times for non-emergency procedures.
Research context – the Virtual Fracture Clinic
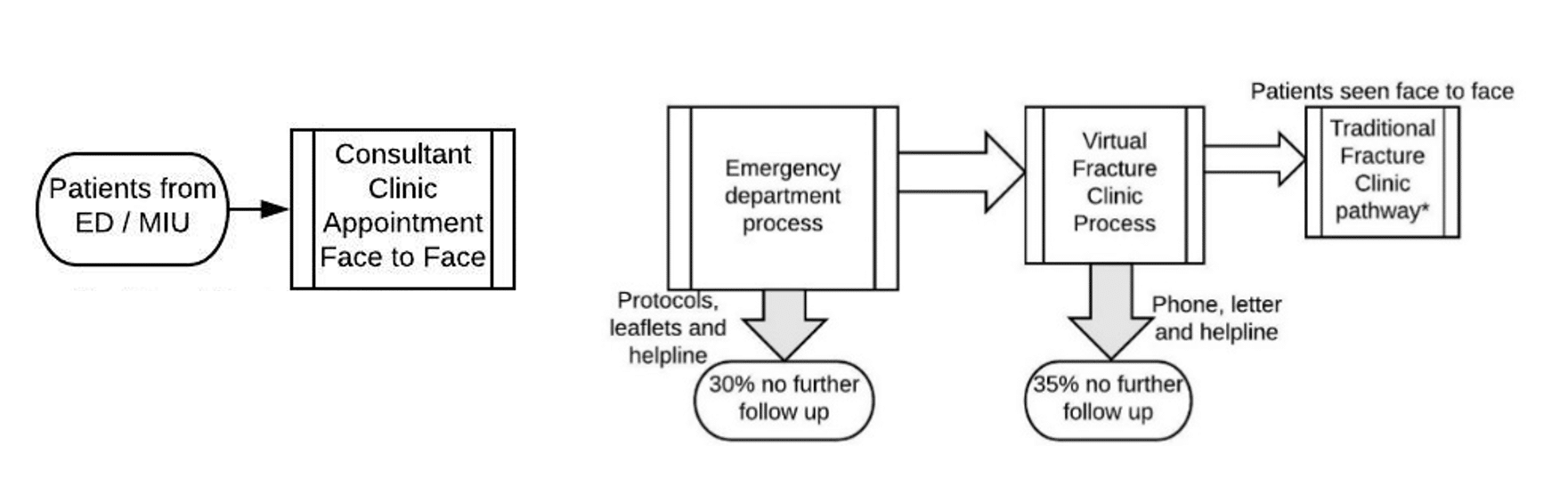
The following case study concerns the redesign of the fracture clinic pathway, termed the ‘virtual fracture clinic’ (VFC), which was developed in the Orthopaedics department at Glasgow Royal Infirmary (GRI) between 2011 and 2014 with the primary aim of improving patient care.
The VFC aims to reduce the unnecessary duplication in a traditional fracture clinic (TFC), in which patients with minor orthopaedic trauma were required, after immediate attendance and treatment at the emergency department, to have a further face-to-face consultation with an orthopaedic clinician, often within 48 hours[5].
The new pathway applies evidence-based standard protocols agreed between the emergency and orthopaedic departments to reduce unnecessary variation.
The use of removable Velcro splints for specific injuries enables direct emergency department discharge of minor stable fractures and facilitates patient self-care without the need to subsequently attend a specialist clinic. Those patients not discharged have their records and X-rays reviewed seven days a week by an orthopaedic consultant and senior nurse in a virtual clinic.
The resulting management plan is agreed with the patient by telephone immediately afterwards. In consequence, patients attend in person only when it is necessary, at the optimal time in their recovery and with the most relevant specialist.
Figure 1 shows the difference between the TFC and the VFC patient pathways.
Figure 1: Illustration of patient pathways in Traditional Fracture Clinic compared with Virtual Fracture Clinic
Although by 2014 the clinical case for the VFC was becoming established, the Scottish Government’s Quality and Efficiency Support Team (QuEST) needed formal evidence of its cost-effectiveness, in order to support the successful diffusion and reliable implementation of this service redesign across NHS hospitals in Scotland[6].
Research
The collaborative research team from the University of Strathclyde, NHS Scotland and The Scottish Government started in 2014. The first step consisted of a careful mapping of both TFC and VFC pathways. Following an extensive data gathering process, involving both already recorded and newly-observed data, two different Discrete Event Simulation (DES) models were built to represent the alternative patient pathways, together with their respective associated resource utilisations and detailed costs.
The models were explicitly designed to reflect variability in costs as not every patient has the same needs. This modelling process enabled stakeholders to gain a clear and agreed understanding of the overall cost effectiveness of the new VFC, in comparison to the TFC.
Box 1: Discrete Event Simulation
Discrete Event Simulation (DES) involves building a visually interactive time based computer model that can mimic important activities and decisions in a process and their interactions. Using DES, one can gain detailed insights into complex stochastic processes as it records performance measures (including flow times and resource utilisations) under realistic operating conditions. Although DES has been widely applied to healthcare modelling [9], its use in bottom-up, micro costing models of virtual clinics is new.
Research insights
Previous research established that there was a 65% reduction in the number of first outpatient face-to-face attendances in orthopaedics due to the VFC (Anderson et al., 2017). In the VFC pathway, the resources required per day were significantly lower for all staff groups. The overall cost per patient for the VFC pathway were 38% lower than for the TFC pathway (Anderson et al., 2017). Evidence of cost savings was paired with knowledge of clinical safety and effectiveness (Jenkins et al., 2016). Patients were also satisfied with the VFC pathway, the information provided and the outcome of their injuries. Overall, this study provides further evidence for the adoption of the new virtual clinic model and serves as a basis for its application in other healthcare settings.
Impacts
The ability of relevant stakeholders and healthcare policy decision-makers to compare the clinical and cost-effectiveness of the new virtual clinic method to the traditional approach had a number of practical impacts, as noted below.
Direct impacts
Use and dissemination of these research insights (Scottish Government, no date) enabled policy-makers from the Scottish government to build a convincing case for the diffusion of the VFC and its implementation in NHS hospitals throughout Scotland.
Further interest in these research insights has reached far beyond the Scottish context through presentations to a stream of national and international visitors to the VFC at GRI, including the Chief Medical Officer for Scotland.
The use and dissemination of these insights has been supported by a publicly available website (Glasgow Royal Infirmary, no date) with a host of features, such as: a patient area, a clear explanation of the new patient pathway, a summary of the evidence underpinning the pathway redesign and the resulting improvement in performance, as well as an extensive set of practical resources for fellow healthcare professionals.
The website also includes a digital map indicating the substantial number of hospitals in Scotland, the wider UK and abroad (around 50 in total) who have fully implemented the VFC concept – in addition to the numerous other hospitals (well over a hundred) who have either visited the VFC at GRI or made enquiries otherwise.
Indirect impacts
There have been a number of additional impacts, ensuring both the further spread of the DES modelling methodology and the continued funding of similar research projects in different healthcare settings.
In the course of this research, 82 staff from the NHS and Scottish Government improvement teams were trained in DES modelling through face-to-face training, hands-on workshops, individualised support, and the development of an online ‘knowledge hub’ (Knowledge Hub, no date) which serves to provide an online forum for discussion and learning about the application of DES.
Moreover, the use of DES in healthcare contexts was disseminated to a wider audience at national symposiums and conferences for healthcare policy makers and practitioners, which has also informed the development of future DES training materials for NHS Scotland.
In addition, 25 Honours and Masters students from Strathclyde Business School have worked on healthcare modelling projects across a range of NHS Boards between 2015 and 2020.
Finally, the successful outcome of the VFC research has helped to support the use of DES modelling for cost effectiveness analysis in subsequent initiatives funded by the Scottish Government, including the development of virtual clinics for elective patient referrals.
Conclusions
In the face of the urgent need for cost effective ways to meet the increasing healthcare needs of the population and improve the service to patients, this case study has exemplified how applied research can directly support healthcare policy makers in introducing new ways of working into their organisations.
The use of DES modelling for cost effectiveness analysis has helped to build a convincing case for the implementation of the virtual clinic method in orthopaedic trauma care across NHS Scotland. The wider dissemination of these insights has ensured the training of healthcare practitioners in the use of simulation modelling, the practical development of the simulation methodology through student placements and projects, and further support for DES modelling for cost effectiveness analysis in different healthcare settings.
More generally, helping NHS Scotland – and healthcare systems globally – to effectively address the urgent cost and other pressures facing them requires research that allows policy makers to make properly informed decisions.
This case study has demonstrated an effective way to determine reliable estimates of policy change by applying an agreed modelling tool in a manner that involves all relevant stakeholders and helps to build their long-term capacity for service redesign and improvement.
You can read the full article here.
[1]National Health Executive (2015) Cost pressures, not demand, the main reason the NHS is struggling, National Health Executive
[2] Scottish Government (2019) Personalising Realistic Medicine: Chief Medical Officer for Scotland’s Annual Report 2017-2018.
[3] Scottish Government (2017) The Modern Outpatient: A Collaborative Approach, 2017 – 2020.
[4] Scottish Access Collaborative (October, 2017) The Scottish Access Collaborative Six Core Principles.
[5] See ‘Cost comparison of orthopaedic fracture pathways using discrete event simulation in a Glasgow hospital’, Anderson, G. H. et al. (2017) BMJ Open, 7(9), pp. 1–12. doi: 10.1136/bmjopen-2016-014509.
[6] Scottish Government (no date) Whole Systems Patient Flow, Quality, Efficiency, and Support Team.
Authors
The Fraser of Allander Institute (FAI) is a leading economy research institute based in the Department of Economics at the University of Strathclyde, Glasgow.